Nanotechnology in medicine
Nanotechnology in Medicine
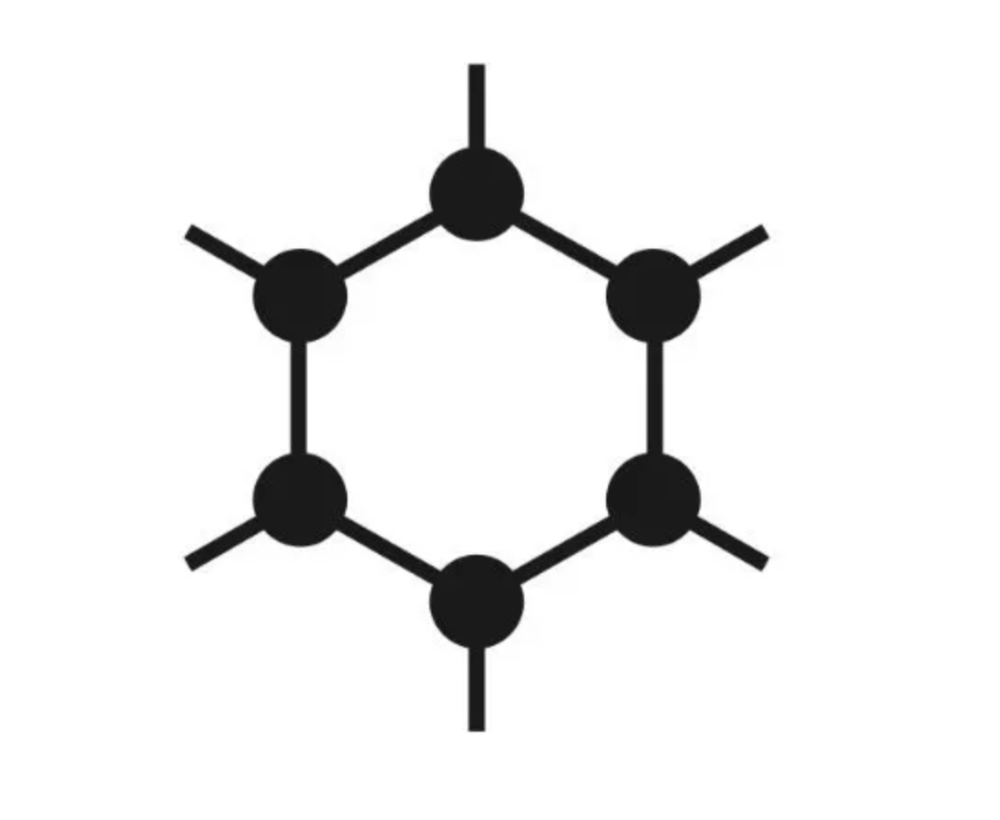
Nanotechnology, the manipulation of matter at the nanoscale (typically 1 to 100 nanometers), has emerged as a revolutionary field in medicine, offering innovative solutions for diagnosis, treatment, and prevention of diseases. Its unique properties, which differ significantly from those of bulk materials, enable the development of advanced medical applications. This essay explores the various applications of nanotechnology in medicine, including drug delivery systems, diagnostic tools, imaging techniques, and cancer treatment, while also addressing the potential challenges and ethical considerations involved.
1. Drug Delivery Systems
One of the most promising applications of nanotechnology in medicine is the development of advanced drug delivery systems. Traditional drug delivery methods often face challenges such as poor solubility, rapid degradation, and nonspecific targeting, which can lead to reduced efficacy and increased side effects. Nanoparticles, due to their small size and large surface area, can overcome these challenges by enhancing the solubility and stability of drugs.
a. Targeted Drug Delivery
Nanoparticles can be engineered to target specific cells or tissues, allowing for more effective treatment with fewer side effects. For example, cancer cells often have unique surface markers that can be targeted by nanoparticles. By attaching antibodies or ligands to the surface of nanoparticles, researchers can create drug delivery systems that selectively bind to cancer cells, releasing the drug only where it is needed. This targeted approach minimizes damage to healthy cells and enhances the overall effectiveness of the treatment.
b. Controlled Release Systems
Nanotechnology also facilitates the development of controlled release systems, where drugs are released in a regulated manner over time. This can improve therapeutic outcomes by maintaining consistent drug levels in the body, reducing the need for frequent dosing. For instance, polymeric nanoparticles can encapsulate drugs and release them in response to specific stimuli, such as changes in pH or temperature, allowing for localized treatment.
2. Diagnostic Tools
Nanotechnology has significantly enhanced diagnostic techniques, leading to more accurate and rapid detection of diseases. Traditional diagnostic methods can be time-consuming and may require large amounts of biological samples. Nanoparticles, however, can be used to create highly sensitive and specific assays that require minimal sample volumes.
a. Nanobiosensors
Nanobiosensors are devices that utilize nanomaterials to detect biological substances at very low concentrations. These sensors can be designed to identify biomarkers associated with various diseases, including cancer, cardiovascular diseases, and infectious diseases. For example, gold nanoparticles can be employed in lateral flow assays, enabling rapid detection of pathogens in clinical samples. The high surface area of these nanoparticles allows for enhanced interaction with target molecules, leading to improved sensitivity.
b. Imaging Techniques
Nanotechnology has also revolutionized imaging techniques, enabling the development of contrast agents that enhance the visibility of tissues and organs. Nanoparticles can be engineered to improve magnetic resonance imaging (MRI), computed tomography (CT), and ultrasound imaging. For instance, superparamagnetic iron oxide nanoparticles can be used as contrast agents in MRI, providing better resolution and contrast compared to conventional agents. This improved imaging capability can facilitate early diagnosis and better monitoring of disease progression.
3. Cancer Treatment
Cancer treatment has greatly benefited from advances in nanotechnology. Traditional cancer therapies, such as chemotherapy, often result in systemic toxicity and resistance. Nanotechnology offers innovative approaches to enhance the efficacy of cancer treatments while minimizing side effects.
a. Nanoparticle-based Therapies
Nanoparticles can be used as carriers for chemotherapeutic agents, delivering the drugs directly to tumor sites while sparing healthy tissues. For instance, liposomes and polymeric nanoparticles have been extensively studied for their ability to encapsulate chemotherapeutic drugs, enhancing their therapeutic index. Additionally, nanoparticles can be designed to release drugs in response to specific tumor microenvironments, such as acidic pH or elevated enzyme levels, ensuring targeted therapy.
b. Immunotherapy
Nanotechnology also plays a crucial role in cancer immunotherapy, where the immune system is harnessed to fight cancer. Nanoparticles can be used to deliver immunotherapeutic agents, such as checkpoint inhibitors or cancer vaccines, enhancing their effectiveness. For example, nanoparticles can be engineered to present tumor antigens, stimulating a robust immune response against cancer cells.
4. Challenges and Ethical Considerations
While the potential of nanotechnology in medicine is immense, several challenges and ethical considerations must be addressed.
a. Safety and Toxicity
The biocompatibility and toxicity of nanoparticles are critical concerns. As nanoparticles interact with biological systems differently than bulk materials, understanding their safety profiles is essential. Long-term studies are needed to assess the potential toxic effects of nanoparticles, particularly their accumulation in the body and potential impacts on various organs.
b. Regulatory Framework
The rapid advancement of nanotechnology in medicine poses challenges for regulatory agencies. Existing regulations may not be adequate to address the unique properties and potential risks associated with nanomaterials. Establishing a comprehensive regulatory framework that ensures the safety and efficacy of nanomedicine products is crucial for gaining public trust and facilitating their clinical application.
c. Ethical Issues
Ethical considerations surrounding the use of nanotechnology in medicine include issues related to informed consent, equity in access to advanced treatments, and potential misuse of nanotechnology for non-therapeutic purposes. Ensuring that patients are fully informed about the risks and benefits of nanomedicine is essential for ethical practice.
Conclusion
Nanotechnology represents a paradigm shift in medicine, offering innovative solutions for drug delivery, diagnostics, and cancer treatment. The ability to manipulate materials at the nanoscale has led to the development of targeted and controlled drug delivery systems, highly sensitive diagnostic tools, and novel cancer therapies. However, addressing the challenges of safety, regulatory frameworks, and ethical considerations is vital for the successful integration of nanotechnology into clinical practice. As research in this field continues to advance, nanotechnology has the potential to transform the landscape of medicine, leading to improved patient outcomes and revolutionizing healthcare.