Morning Migraines
What triggers morning migraines? Scientists might now know. Mood, stress, energy, and poor sleep, can all be indicators of a morning migraine the next day, a new study finds. It could help some migraine sufferers predict—and maybe even prevent—their next one.

For many important life events, festivals, and ceremonies—including her own wedding—software engineer Katyayani Vajpayi endured a throbbing migraine that occurred mainly on the left side of her head, making her nauseous, and disturbing her vision. Sometimes the pain is so paralyzing she just wants to stay home alone, curled up in bed in a dark room.
Vajpayi is not alone. At least one in 10 people globally suffer from migraine headaches at some stage in their lives. This is likely an underestimate as three times more women than men, and more poor people than rich, suffer from migraines. Even when treated, therapies are not very effective, especially after the migraine has already started.
"The headache would just attack without any warning. I wished I could see them coming," says Vajpayi. "At least I would have been better prepared."
Now, a new study published in the journal Neurology shows that smartphone apps or diaries that can track sleep, behavior, and emotional states, can predict headaches in some patients. The study found that people with a morning migraine reported lower energy levels the previous day and poorer quality sleep the night before.
"If people do track their energy levels, physical activity, and sleep over time, they may be able to identify how some of these may be related to headache attacks," says Kathleen Merikangas, a psychiatrist and epidemiologist at the National Institute of Mental Health in Bethesda, MD, who led the study.
The study shows that tracking sleep and other triggering factors may not only predict headaches in some patients, but it might also help develop tools to prevent them.
"The findings suggest that changes in the body and brain are already taking place before a person first feels a headache,” Monica Bertagnolli, the director of the National Institutes of Health, wrote in a blog post.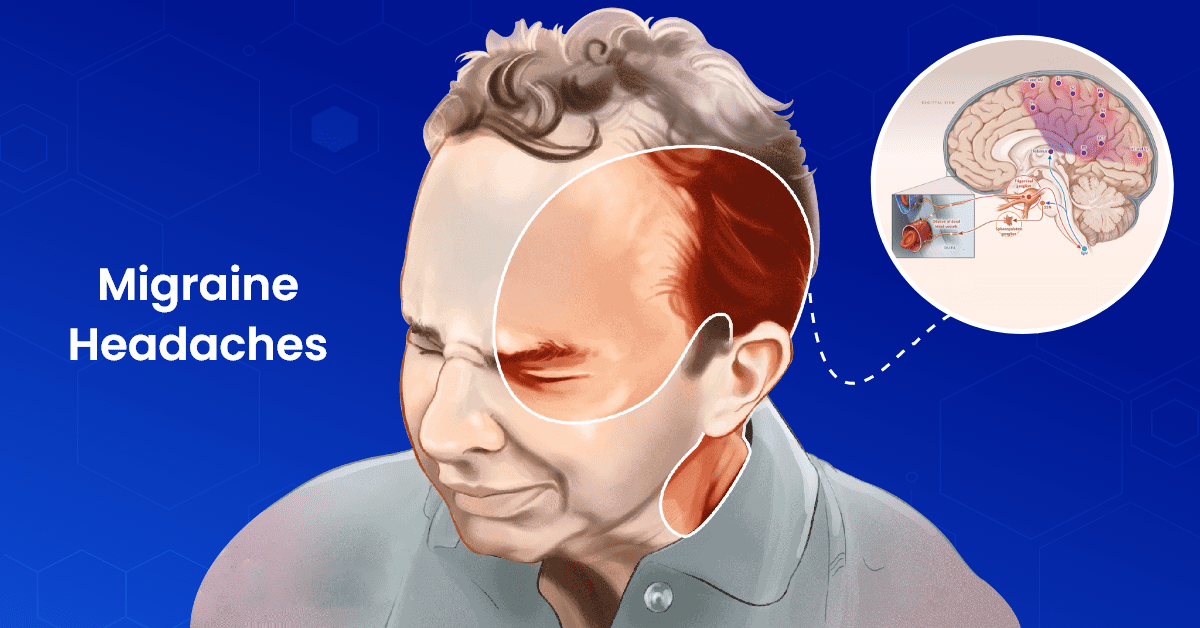
Migraine is a complex disease
Migraines are much worse than bad headaches.
Most patients feel a frequent and severe throbbing pain on one side of the head. Although migraines can occur any time of the day, they commonly occur in the mornings upon waking.
Some people experience migraines at predictable times, such as before menstruation, following a stressful week of work, or on weekends when regular sleep habits are disturbed; others are hit with the pain with no obvious warning.
The first phase of migraine, called prodrome, can begin up to 24 hours before the actual headache. This period might be punctuated by food cravings, unexplained mood changes—such as depression or euphoria—lack of sleep, uncontrollable yawning, or increased urination.
In some patients, neurological disturbances called migraine aura can occur before or during the migraine headaches. The aura can be dizziness, a ringing in the ears, zigzag lines disrupting clear vision, nausea, vomiting, or sensitivity to light and sound. While aura can be a warning sign of an impending migraine attack, it can also occur at the same time as the throbbing headache. Not all patients who suffer migraines, however, experience an aura.
After the migraine headache subsides, the postdrome stage or a migraine hangover follows. This phase, which can last anywhere from a few hours up to 48 hours, is characterized by fatigue, difficulty concentrating, dizziness, weakness, and low energy. To some, the postdrome really feels like an alcohol-induced hangover, after which the whole cycle can repeat immediately. Or, an individual can be symptom-free between attacks.
A migraine is believed to occur after the abnormal triggering of a specific nerve and its associated blood vessels on the surface of the brain—but the exact cause is not yet known. In fact, there are many other migraine triggers and very few treatments are based on any specific mechanism.
"If you identify the risk factors that are personal to you and make lifestyle adaptations to accommodate them, then you can reduce the incidence of headaches," says Donald Penzien, a headache and pain specialist at Wake Forest School of Medicine in Winston-Salem, NC.
Tracking sleep to prevent headaches
To find out how the risk of developing headaches is linked to an individual’s mood, sleep, energy, or stress level, scientists recruited 477 volunteers in Washington, DC, and surrounding areas. The volunteers, aged seven to 84, included 186 males and 291 females with or without a history of migraine.
Through a smartphone app, they were asked to track their anxiety, mood, energy, stress, and headaches, four times each day for two weeks. Each morning, volunteers also reported on the quality of their sleep the night before, which was also measured via a wearable device.
The scientists then compared the first incidence of headache among those who had a history of migraines with those without.
The study found that someone had a greater chance of developing a morning headache if they did not sleep well the night before or had reported lower energy the day before.
This study is impressive in not only the large number of people studied at a wide range of ages, but also in the much higher percentage of men included, which is unusual for many migraine studies, says Jelena Pavlovic, a migraine specialist at the Montefiore Medical Center in Bronx, NY.
To the surprise of the study authors, afternoon or evening headaches were not caused by poor sleep quality or lower energy the day before. Instead, these were more likely linked to higher stress levels or higher-than-average energy the day before.
"Disturbed sleep is a setup for morning attacks the next day, while higher stress levels and higher energy are likely to drive the afternoon attacks," says Pavlovic.
The study didn’t find any connection between feeling anxious or depressed and headaches the next day, so long as the sleep or energy levels were not disturbed.
The study shows that symptoms of a migraine, particularly nausea and vomiting, may interfere with sleep. However, it did not include some of the dietary and hormonal factors that may trigger headache attacks. The finding that migraine attacks are also associated with diminished energy on the previous day suggests that some physiological changes may occur prior to sleep onset that induce poor-quality sleep. However, it is not yet clear whether sleep disruption is a trigger or a symptom of migraine. "We are now doing overnight sleep EEG monitoring to try to address this question,” says Merikangas.
But the study confirms, what many migraine sufferers learn from experience: regular eating, drinking, sleep, and physical activity, can reduce the chance of headache.

"This study reaffirms that one of the most effective treatments for migraine is a regular good night's sleep," says Pavlovic. While some migraine attacks are unavoidable in patients, the earlier someone can treat their headache, generally, the shorter and less burdensome their symptoms would be, says Pavlovic.
"While the benefits of tracking and predicting migraine attacks can seem modest, frankly, they're on par with a lot of other treatments in terms of being able to at least prevent or reduce the likelihood of headache," says Penzien.
Source
https://en.wikipedia.org/wiki/Migraine
https://www.medicalnewstoday.com/articles/waking-up-with-a-migraine#:~:text=Waking%20up%20with%20a%20migraine%20is%20a%20common%20occurrence.,other%20times%20of%20day%20too.
https://health.clevelandclinic.org/waking-up-with-migraine
https://www.healthline.com/health/migraine/waking-up-with-a-migraine
https://www.sleepfoundation.org/physical-health/morning-headaches
































































